Overview
The Department of Radiation Oncology’s medical residency program is among the longest running of its kind in the country and provides trainees with the clinical and procedural skills necessary to become competent and compassionate radiation oncologists. Our medical residents work in tandem with attending faculty, medical physicists and medical physics residents to pursue research interests and translate these findings to enhance care delivery.
Mission
Our mission is to provide comprehensive training in all aspects of clinical radiation oncology, medical physics, cancer biology and research.
We do this by caring for the diverse population in our immediate area and beyond through innovation in service, research and education.
The radiation oncology residency program:
- Educates residents to be clinically well prepared to practice radiation oncology in academic, hospital or community-based practices.
- Provides residents a fundamental understanding of evidence-based medicine to prepare them for board exams.
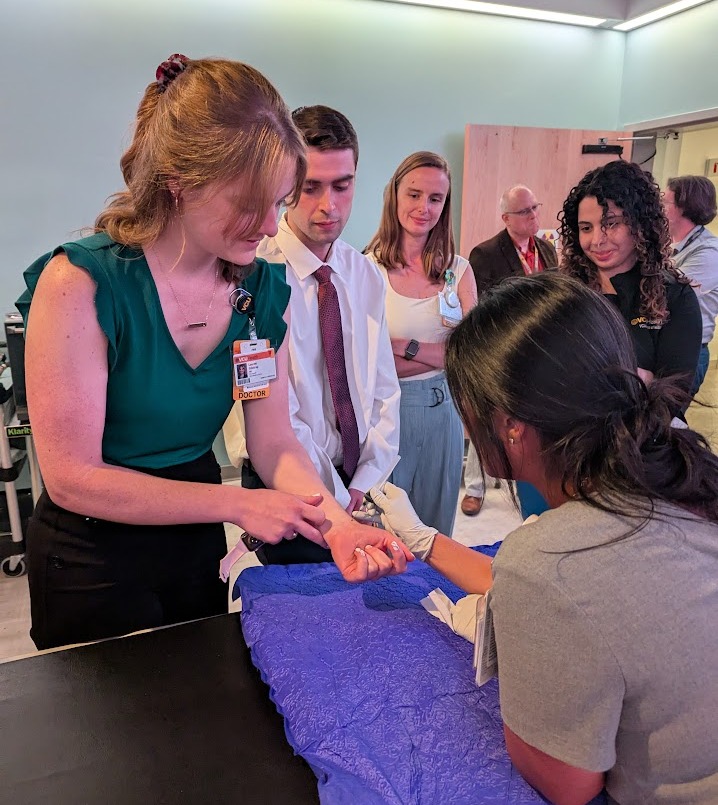
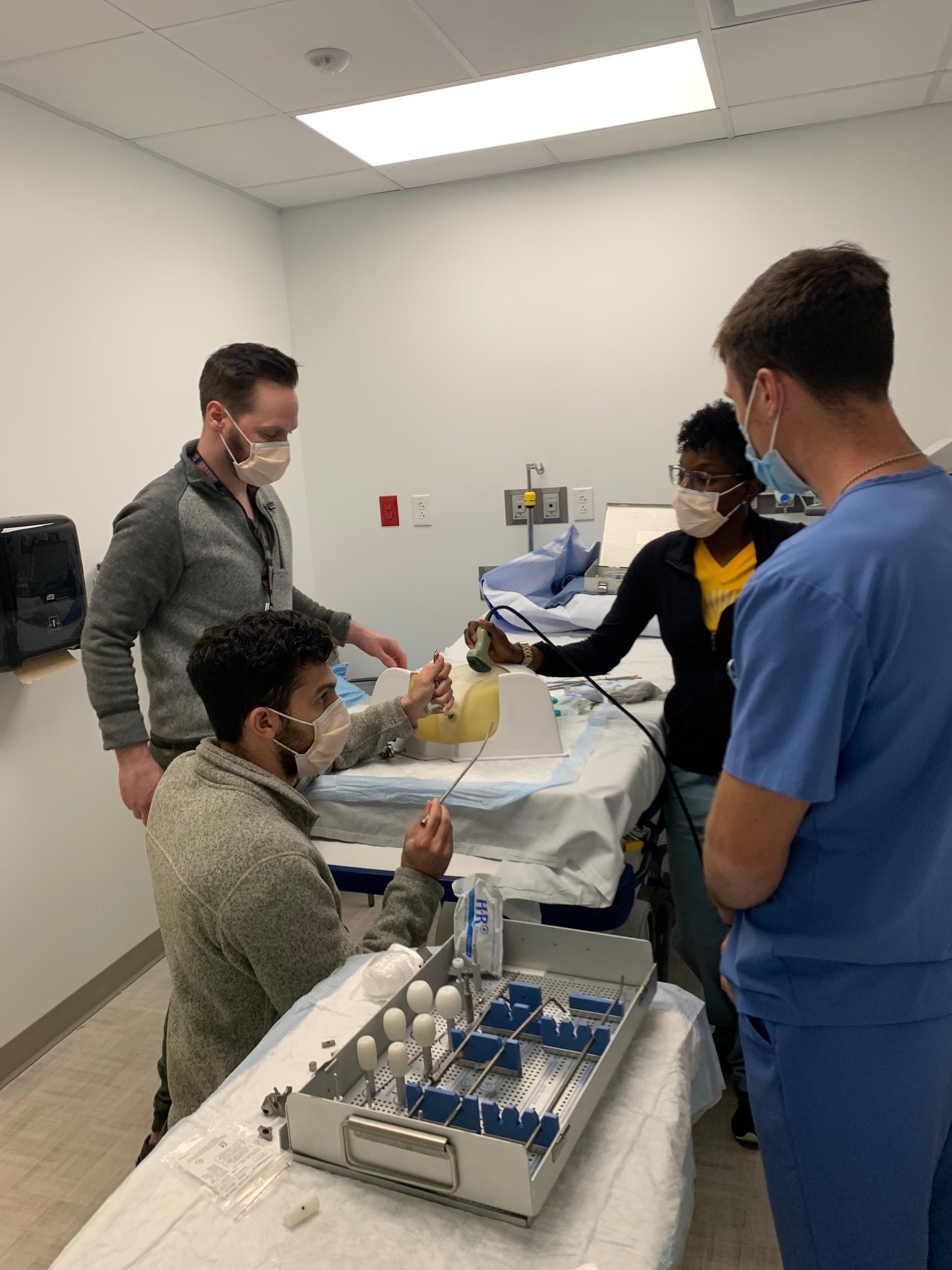
- Develops proficient brachytherapy techniques that will prepare them for a career in procedural radiation oncology.
- Expands residents’ understanding of research to develop skills that will allow for publication and presentation of results.
Discover the Department of Radiation Oncology
Curriculum
Before beginning rotations, incoming PGY-2 residents will participate in the Introductory Radiation Oncology Curriculum (IROC) to prepare for clinical duties.
They remain under the guidance of our attendings during the entirety of their training, with gradually increasing expectations of responsibility.
- Head and Neck
- Gastrointestinal / Gynecological
- Breast
- Central Nervous System
- Pediatrics
- Genitourinary / Prostate
- Thoracic
Additionally, each resident completes rotations at Central Virginia VA Health Care System.
Residents gain exposure to a broad spectrum of oncology patients and their treatments, including the following:
Intensity modulated radiation therapy (IMRT)
- Stereotactic body radiotherapy (SBRT)
- Stereotactic radiosurgery (SRS)
- Image-guided radiation therapy (IGRT)
- Three-dimensional conformal radiation therapy (3D CRT)
- Four-dimensional conformal radiation therapy (4D CRT)
- Deep inspiration breath hold (DIBH)
- Total body irradiation (TBI)
- Low-dose rate (LDR) brachytherapy for prostate malignancies
- High-dose rate (HDR) brachytherapy for breast, gynecologic and prostate malignancies
- Brachytherapy for other malignancies including sarcoma, skin and gastrointestinal malignancies
- Pediatrics
- LDR brachytherapy for pancreatic cancer
In addition to core rotations, residents have the opportunity to supplement their pediatrics training with a one-month rotation at St. Jude Children’s Research Hospital in Memphis, Tennessee, one of the nation’s leading children’s hospitals in the diagnosis and treatment of pediatric malignancies.
Didactics
Resident training includes dedicated, structured and protected education time. Residents and faculty collaborate to present site specific didactic sessions which include hands-on workshops, case presentations and discussions, journal club, guest speakers and visiting professors.
 Radiation physicists and radiation biologists teach formal curriculum throughout the year, and guest speakers from other departments and divisions bring interdisciplinary education to didactics.
Radiation physicists and radiation biologists teach formal curriculum throughout the year, and guest speakers from other departments and divisions bring interdisciplinary education to didactics.
Residents are also expected to attend specialty-specific tumor board reviews, journal club, morbidity and mortality conferences and quality assurance peer review chart rounds.
Additionally, our residents prepare for the oral board exam with an annual mock version of the test. Each resident completes a simulated oral board day, going through various clinical cases in each of the core disease sites tested on the official oral exam. Residents have the chance to acclimate to the setting, and receive feedback and continual preparation leading up to oral boards.
Research Opportunities
Under the guidance and supervision of the Resident Research Committee, residents will spend six months in a research rotation in clinical oncology, medical physics or radiobiology.
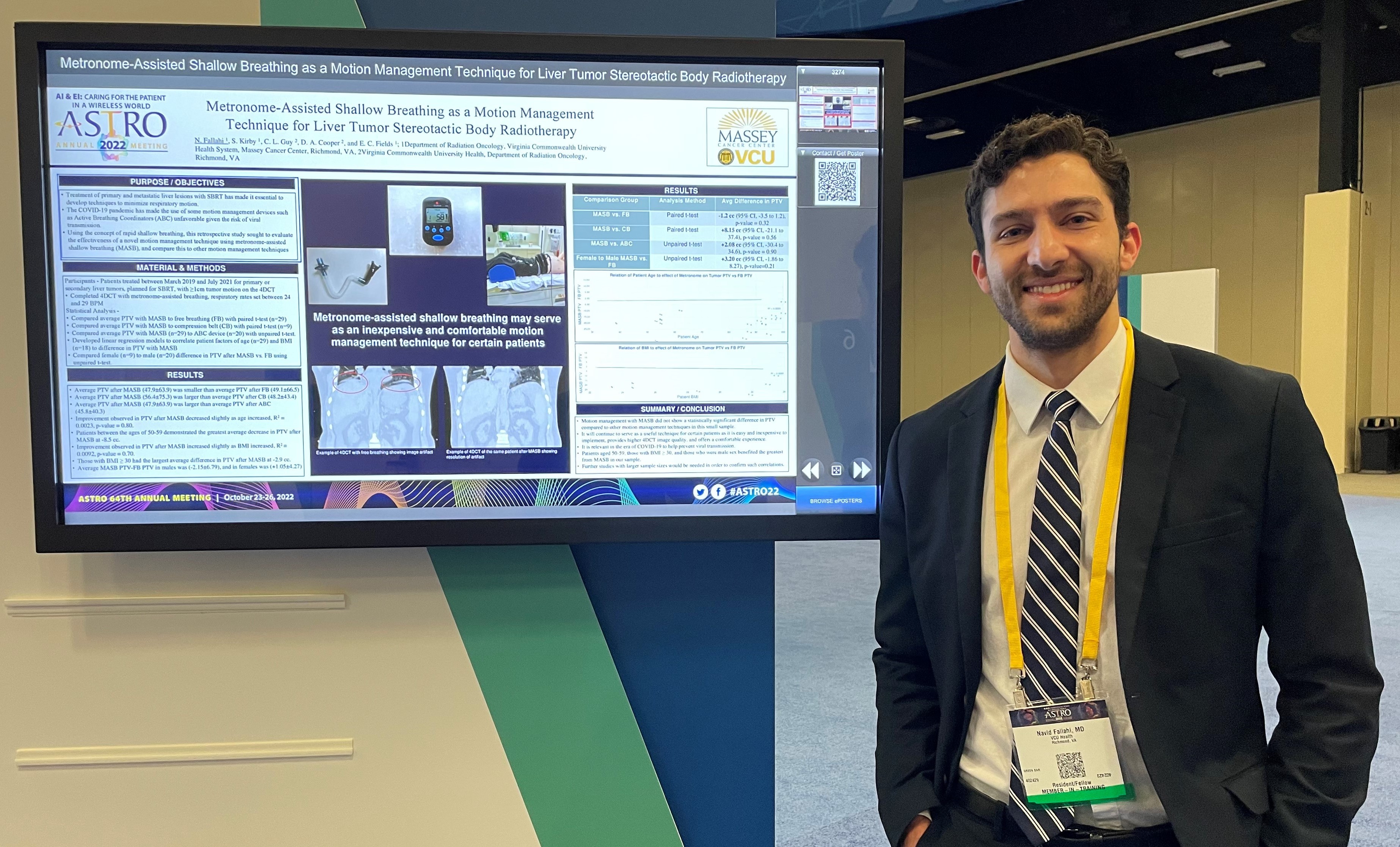 Residents spend six months on research rotations with the possibility to extend. Project results should be submitted for publication in peer-reviewed scholarly journals or presentations at scientific meetings and conferences.
Residents spend six months on research rotations with the possibility to extend. Project results should be submitted for publication in peer-reviewed scholarly journals or presentations at scientific meetings and conferences.
Resident Life
A healthy work-life balance
While our residents work and train, we encourage them to maintain a healthy work-life balance and take advantage of the many activities the Richmond area has to offer. Outdoor adventures like hiking and whitewater rafting are available right here in the city along with museums, a thriving arts scene, live music, craft breweries and cideries, local restaurants boasting national accolades and an abundance of southern charm. Richmond is also situated within a short drive to the beach, the mountains and Washington, D.C., making daytrips and weekend excursions easily accessible.
Learn more about RichmondResident Recruitment
The Department of Radiation Oncology participates in the National Resident Matching Program (NRMP).
All residents must have completed a clinical PGY-1 in an accredited graduate medical education program.
Contract and benefit information
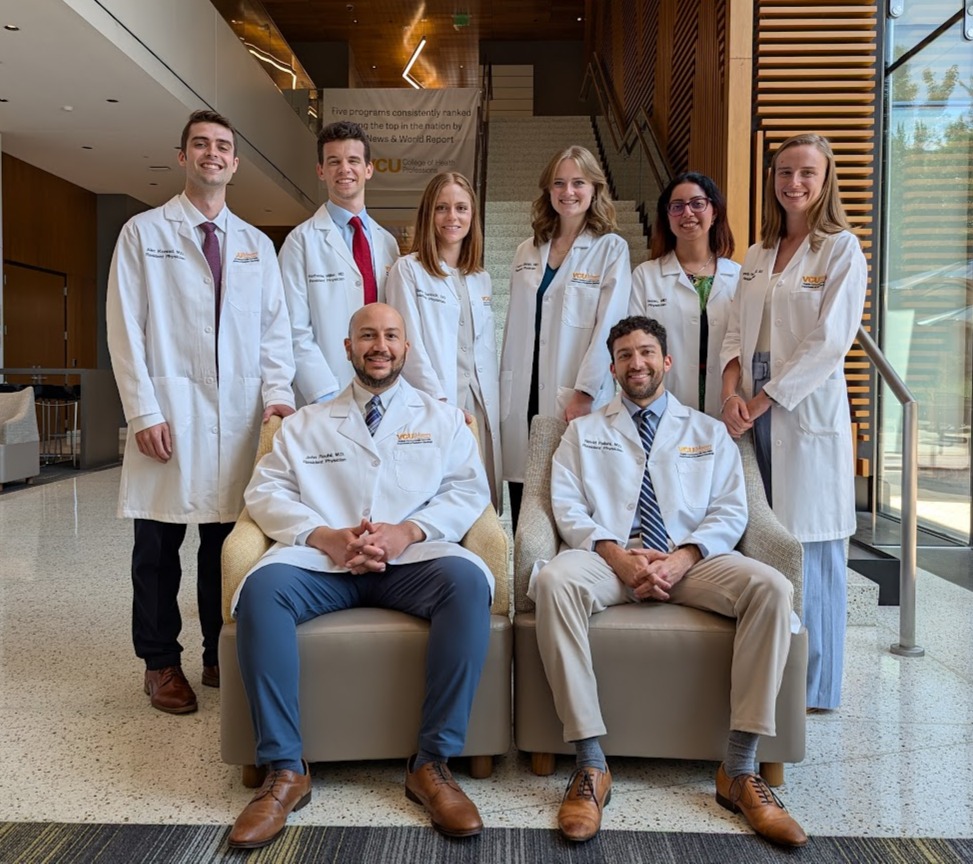
Current Residents
Meet our current Radiation Oncology Clinical Residency Program residents
PGY - 5
Navid Fallahi, MD
Radiation Oncology Chief Resident
Navid Fallahi, MD
Radiation Oncology Chief Resident
Radiation Oncology
BS – Physiology, University of Arizona
MPH – Columbia University
MD – St. George’s University School of Medicine
Internship – Virginia Commonwealth University

John Roubil, MD
Radiation Oncology Chief Resident

John Roubil, MD
Radiation Oncology Chief Resident
Radiation Oncology
BA – International Studies, American University
MD – University of Massachusetts Medical School
Internship – University of Massachusetts Medical School
PGY - 4

Eliane Garlock, DO
Radiation Oncology Clinical Resident

Eliane Garlock, DO
Radiation Oncology Clinical Resident
Radiation Oncology
BS – Biochemistry and Molecular Biology, Bob Jones University
DO – Edward Via College of Osteopathic Medicine – Carolinas
Internship – Mountain Area Health Education Center
PGY - 3
Evrosina Isaac, MD
Radiation Oncology Clinical Resident
Evrosina Isaac, MD
Radiation Oncology Clinical Resident
Radiation Oncology
BS – Biomedical Engineering, Virginia Commonwealth University
MD – Virginia Commonwealth University
Internship – Virginia Commonwealth University
Nathaniel Miller, MD
Radiation Oncology Clinical Resident
Nathaniel Miller, MD
Radiation Oncology Clinical Resident
Radiation Oncology
BS Kinesiology and Health Sciences, College of William and Mary
MD – Virginia Commonwealth University
Internship – Riverside Medical Center
PGY - 2
Lauren Gilstrap, MD
Radiation Oncology Clinical Resident
Lauren Gilstrap, MD
Radiation Oncology Clinical Resident
Radiation Oncology
BS – Biology, University of Georgia, Athens
MD – Medical College of Georgia at Augusta
Internship – Transitional Year Piedmont Athens Regional

Alec Konrad, MD
Radiation Oncology Clinical Resident

Alec Konrad, MD
Radiation Oncology Clinical Resident
Radiation Oncology
BS – Biology, Wofford College
MD –Joan C. Edwards School of Medicine at Marshall University
Internship – Internal Medicine Marshall University

Amanda Pomeroy, MD. MS
Radiation Oncology Clinical Resident

Amanda Pomeroy, MD. MS
Radiation Oncology Clinical Resident
Radiation Oncology
BA – Biology University of Vermont
MS – Biomedical Sciences Tufts University School of Medicine
MD – Tufts University School of Medicine
Internship – Internal Medicine Duke University
Photogallery
Contacts
Emma C. Fields, MD
Program Director
Emma C. Fields, MD
Program Director
Radiation Oncology
Twitter: @emmacfields
Email: Emma.Fields@vcuhealth.org
Jo Lombardi
Program Coordinator